SUNRISE Research – abstract –のご報告
去る6月1日、愛知県名古屋において、「海外学会にsubmitする前の抄録を複数の査読者で添削する」という新しい試みをOrbus Neich®のご協力のもと行いました。対象の学会としては、最難関のひとつであるAHAを選択しました。事前に東海大学伊刈教授とSUNRISE林田による添削を行い、オンサイトでは中澤、重城および原の3名と、お招きした高木健督先生(大垣市民病院)、田中哲人先生(名古屋大学)を含めた総勢10名を超えるドクターで熱いディスカッションを行いました。
今回abstractを持ち寄っていただいた精鋭は、
根岸 陽輔先生(岡崎市民病院)
吉岡 直輝先生(大垣市民病院)
柴田 直紀先生(一宮市民病院)
大森 寛行先生(岐阜ハートセンター)
朴 美仙先生(島根大学)
の5名であり、それぞれ非常に個性的でclinically relevantな素晴らしい内容でした。
最終的にmodifyしたものをsubmitしていただいた結果、根岸先生、大森先生および朴先生の3名のabstractが見事採択されました!もちろん修正前のものはsubmitしていないので、修正の貢献度は不明ですが、60%の採択率はgreatですね。
11月のChicagoでの発表は改めてご報告させていただきます。乞うご期待。
次はあなたの街に伺いますよ。
Abstracts
根岸先生 (ポスター11/11/2018 10:30AM)
Contrast-induced nephropathy and long-term clinical outcomes following percutaneous coronary intervention in patients with advanced renal dysfunction (estimated GFR ‹ 30)
Background: The incidence of contrast-induced nephropathy (CIN) increases with the progression of renal dysfunction. Therefore, percutaneous coronary intervention (PCI) are frequently avoided in patients with advanced renal dysfunction due to fear of CIN, which may result in poor outcomes. On the other hand, recent reports have shown that PCI can be safely performed even in patients with advanced renal dysfunction by instituting appropriate CIN-prevention strategies. However, data are limited regarding the occurrence and prognostic influence of CIN in patients with advanced renal dysfunction.
Methods: We examined the data obtained from 323 consecutive patients with advanced renal dysfunction (estimated glomerular filtration rate [eGFR] ‹30 mL/min/1.73 m2) who underwent PCI at 5 hospitals between 2011 and 2016. CIN was defined as a ≥25% increase in baseline serum creatinine levels and/or a ≥0.5 mg/dL increase in absolute serum creatinine levels within 72 h after PCI. Incidence of all-cause death and the initiation of permanent dialysis were examined during follow-up.
Results: The prevalence of emergency/urgent PCI was 53.3%. Intravascular ultrasound was used in 266 patients (82.4%), and the volume of contrast used was 71.7±57.2 mL. CIN was observed in 31 patients (9.7%). Patients who developed CIN more commonly presented with shock and pulmonary congestion and received emergency/urgent PCI and had received a greater volume of contrast agent. The median follow-up duration was 656 days (interquartile range 257–1143 days). The cumulative rates of all-cause death or the initiation of permanent dialysis, all-cause death, and the initiation of permanent dialysis were 38.1%, 25.9%, and 18.2%, respectively at 2 years. A comparison between patients with and without CIN showed no significant intergroup differences in the occurrence of the aforementioned events.
Conclusions: The development of CIN was not a common occurrence if PCI was performed by instituting appropriate CIN-prevention strategies even in patients with advanced renal dysfunction. The long-term prognosis following PCI is observed to be poor in this studied population.
大森先生 (ポスター11/10/2018 2:15PM)
Use of Mid-distal, rather than Far-distal, Measurement of Computed Tomography-Derived Fractional Flow Reserve for More Accurate Evaluation of Ischemic Status
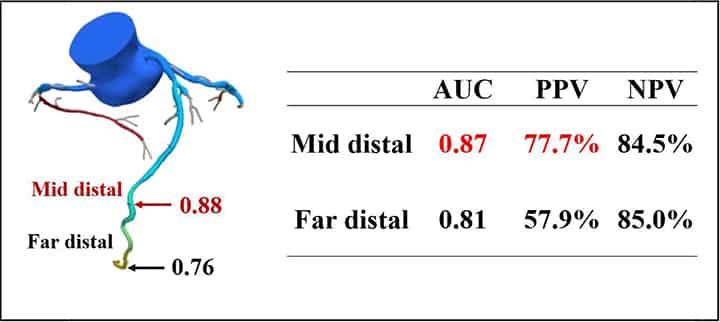
Introduction: Computed tomography-derived fractional flow reserve (FFR-CT) has recently been introduced in clinical settings as one of the novel coronary imaging technologies. However, the ideal position for FFR-CT measurements is unknown.
Hypothesis: The ideal position for FFR-CT measurement should be at the mid-distal site, where the distal sensor of the invasive fractional flow reserve (FFR) wire is expected to be placed, as far-distal FFR-CT measurements may overestimate the presence of ischemia.
Methods: The FFR-CT and invasive FFR values were assessed prospectively in 390 vessels (luminal stenosis in coronary CT ≥50%) in267 patients at our institution. FFR-CT was measured at far-distal and mid-distal (Figure), where the distal sensor of the invasive FFR wire is expected to be placed. The predictive accuracies of mid-and far-distal FFR-CT were compared using the DeLong method of area under the curve (AUC) of the receiver-operating characteristics by setting invasive FFR of ≤0.80 as objective variable. The positive and negative predictive values of FFR-CT of 0.80 were also evaluated.
Results: The median age of the patients was 71 years, and 65.5% of the patients were men. The AUC of the mid-distal FFR-CT was greater than that of the far-distal FFR-CT (0.87[95% CI,0.83–0.90]vs 0.81[95% CI,0.76–0.85], p ‹0.001). The positive predictive value (PPV)of the mid-distal FFR-CT was also better than that of the far-distal FFR-CT (77.7% vs 57.9%), whereas the negative predictive values (NPV) were comparable between the mid-and far-distal FFR-CT (84.5% vs 85.0%). These tendencies were common when coronary arteries were evaluated in each.
Conclusions: The far-distal FFR-CT over estimated the presence of ischemia as compared with the invasive FFR. Mid-distal FFR-CT is more accurate than far-distal FFR-CT, and FFR-CT should be measured at the mid-distal site, where the distal sensor of the invasive FFR pressure wire is expected to be placed.
朴先生 (ポスター11/11/2018 10:30AM)
Delirium is associated with high mortality in octogenarian patients with acute decompensated heart failure
Introduction: Delirium is associated with high mortality in elderly patients who undergo cardiac surgery, partly owing to difficult management with negative hemodynamic aspects of antipsychotics. However, the prognostic impact of delirium in elderly patients with acute decompensated heart failure (ADHF) and the factors associated with delirium are unclear.
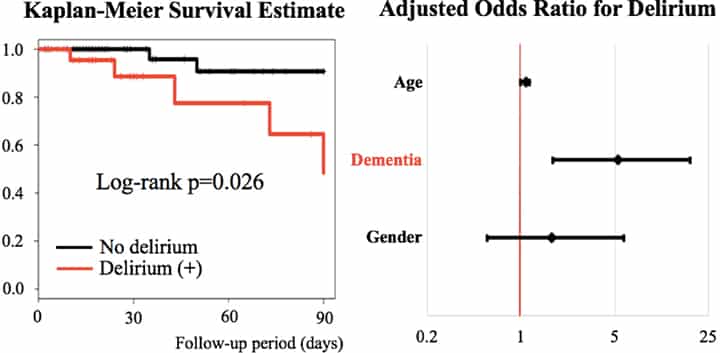
Hypothesis: Delirium has a negative prognostic impact in octogenarian patients with ADHF.
Methods: This prospective observational study enrolled 75 consecutive patients admitted with ADHF between January 1 and May 31, 2018, at our institution. To assess the prognostic impact of delirium, the patients were classified into two groups according to the presence of delirium during hospitalization diagnosed using DSM-5. The primary end point was 3-month all-cause mortality from the time of hospitalization. The difference in survival was evaluated using a log-rank test; and the prognostic impact of delirium, using a multivariable Cox regression analysis. Factors associated with delirium during hospitalization were also assessed using a multivariable logistic regression analysis.
Results: The patients’ median age was 82 years. The proportions of men and those with ischemic heart disease as the etiology of ADHF among the subjects were 53% and 37%, respectively. During hospitalization, delirium occurred in 26 patients, and 3-month survival was statistically different between the patients with and those without delirium (48.5% vs 90.8%, p=0.026). Delirium was associated with high mortality (adjusted hazard ratio, 95% confidence interval [CI]: 7.0, 1.0–48.7; p=0.049). Factors associated with delirium included history of dementia (adjusted odds ratio, 95% CI: 5.3, 1.7–18.3; p=0.005).
Conclusions: Delirium was associated with high mortality in octogenarian patients with ADHF. We discuss the possible management and preventive strategies of delirium at presentation.